AI Rivals Doctors at Spotting Prostate Cancer
The PAIR-1 trial conducted with NHS hospitals has found that Lucida Medical’s Pi AI program could detect prostate cancer with roughly the same accuracy as expert radiologists.
Prostate Cancer: A Growing Health Crisis
According to data from the National Institute for Care Excellence, around one in six to eight people assigned male at birth will be diagnosed with prostate cancer in their lives, making it the most common cancer affecting men in the UK today. This number increased steadily—in 2024 alone, over 54,000 new cases of prostate cancer were diagnosed, and Cancer Research UK estimates this number could rise to 85,100 by 2040.
As with most forms of cancer, early detection is key to maximizing patient survival and reducing the long-term impact on quality of life. However, prostates are not routinely screened for malignancy unless the patient exhibits symptoms of enlargement (such as excess urination or sexual dysfunction) or if they are over the age of 50 and specifically request it.
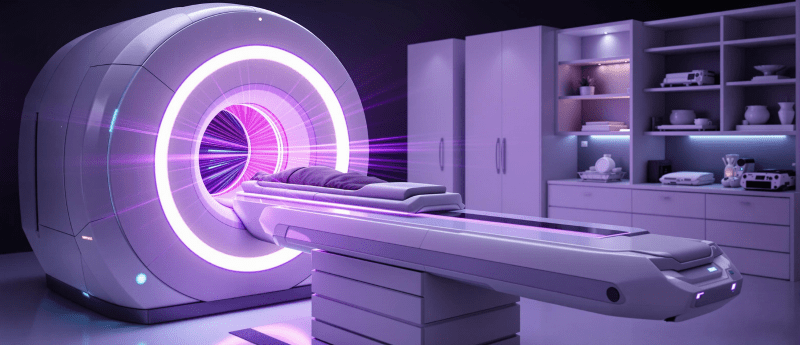
Prostate cancer screening typically involves the patient undergoing a blood test to investigate the levels of prostate-specific androgen, as well as a prostate examination. If the findings from either are particularly concerning, they may be referred for a Magnetic Resonance Imaging (MRI) scan to search for malignancy. If evidence of a tumor is seen on the scan, patients will usually undergo a prostate biopsy.
Prostate MRIs are fast and painless procedures that have been proven to avoid the discomfort and inconvenience of unnecessary biopsies for cancer-free patients. For those with suspicious lesions, MRI images are invaluable for further investigation and determining treatment approaches.
Worldwide Radiologist Shortages
Unfortunately, there is a serious and worsening shortage of radiologists in the NHS. The shortfall currently stands at 30%—a number that is expected to rise to 41% in just five years. As a result, fewer doctors are available to interpret MRI scans, which require significant time and expertise for accurate analysis.
On an international scale, the distribution of radiologists is uneven, with higher-income countries having more radiologists per capita than lower-income countries.
In lower-income countries, there is an average of 794 radiologists per 697 million people—less than two radiologists per million people. Whereas, in countries such as the U.S., Japan, Europe, and the UK, there are approximately 97.9 radiologists per million people. Even then, this number is still insufficient to meet demands.
According to the World Health Organization, by 2050, 22% of the global population will be over the age of 60, increasing the demand for radiologists and imaging services. Our aging population necessitates technological support, as the current workforce alone cannot meet growing healthcare demands.
Prostate Intelligence
To combat this rising issue, Lucida Medical —formerly Cambridge AI Health— developed Prostate Intelligence (Pi), a machine learning software designed to help identify malignancies from prostate MRI scans. It does this by producing three main data outputs from images:
- Cancer Risk Calculation – creating a score on the likelihood of cancer to help minimize the number of patients inappropriately referred for biopsy and prioritizing those in need of urgent investigation.
- Lesion Identification – delineating all concerning areas to ensure no lesions are missed when conducting sampling and treatment.
- Prostate Segmentation – sectioning the image to assist human annotation, analysis, and treatment decisions.
The PAIR-1 trial
The Prostate AI Research-1 (PAIR-1) trial is a retrospective, non-inferiority study, meaning it uses historic data to test whether one method, i.e., Pi, is as effective as another, i.e., traditional multidisciplinary team-(MDT)-backed radiologist interpretation.
The PAIR-1 trial was sponsored by Hampshire Hospitals NHS Foundation Trust to develop and assess the accuracy of the Pi programme. This sponsorship reflects the trust’s commitment to addressing radiologist shortages and improving diagnostic efficiency through AI, ensuring faster and more accurate prostate cancer detection.
As part of this effort, researchers compiled scans from NHS hospitals (2018–2022) and integrated them with images from the PROSTATEx archive , creating a comprehensive dataset for analysis.
While most scans in the trial were used to train and develop the AI, images from 252 patients were kept separately from the rest of the dataset. These images were specifically used to validate the accuracy of Pi’s findings by comparing them with the assessments of an MDT-supported radiologist and the patient’s final diagnosis post-biopsy. Scans that the radiologists had deemed as not requiring biopsy were assumed to be cancer negative for the purposes of the study.
Pi was able to diagnose clinically significant prostate lesions in this cohort with a sensitivity of 95%, compared with the radiologists’ 99%. This difference was within the bounds of the study’s 10% non-inferiority margin. Thus, the study concluded that Pi’s performance matched that of the radiologists.
The researchers added that while these results are promising, the next step in Pi’s validation could be testing the model in a larger sample size to support a narrower non-inferiority margin.
So, Could Pi Replace Radiologists?
Though PAIR-1 showed that Pi could identify prostate lesions at an impressive rate, it did technically have a lower sensitivity than the radiologists; in this trial alone, the AI missed 13 more lesions than human interpreters. Such findings suggest that Pi does not quite match the accuracy of existing NHS radiologists, as not identifying cancer in real patient scans could have catastrophic consequences.
It was also emphasized that “optimal image quality” was required for the AI to perform its analysis, a luxury that may not be possible for doctors making real-time decisions on patient care based on whatever images are available. Finally, the trial acknowledged the possibility that some patients who were referred for scans but did not undergo biopsy may have had cancerous lesions that were missed by their radiologists. This would mean that there may have been patients whose lesions had not been accurately labelled in the validation set, potentially impacting both the sensitivity and specificity of the results.
Recognizing the limitations above, the study authors reported that Pi should not be used as an independent diagnostic programme but rather as a “decision-support tool” to be combined with each radiologist’s clinical experience and the patient’s overall clinical picture.
A Place for Pi
Pi has been labelled as a “diagnostic aid providing a secondary read” by the Royal College of Radiologists, i.e., while it cannot outperform humans, it can certainly assist them by working like a second pair of (highly specialized) eyes during scan interpretation. Mark Hinton, Lucida Medical’s Chief Technology Officer, also stated that Pi was developed to “automate key steps like outlining lesions and calculating risk scores”, saving valuable time when making treatment decisions and plans.
Consultant Radiologist and PAIR-1 Chief Investigator Aarti Shah noted:
“Analyzing MRI scans is a time-consuming task for expert radiologists, and there are too few of us in the UK and in many other countries. Pi offers exciting potential as an aid to help reporting radiologists in triaging workloads, as well as producing visual reports, to aid contouring of lesions for biopsy.”
Based on the PAIR-1 trial and statements from the team, it appears that while Pi may not be a substitute for trained doctors, it could be a valuable asset for validating human interpretation and assisting with the complexity of planning treatment. Such technology could represent a step forward in supporting accurate cancer diagnosis whilst helping avoid invasive medical procedures, reducing workloads for radiologists across the NHS.