Enhancing CAR T-cell therapy for leukemia
A team of scientists from St. Jude Children’s Research Hospital (TN, USA) are transforming the fight against acute myeloid leukemia (AML) in children by using AI to redesign chimeric antigen receptor (CAR) T-cell therapy.
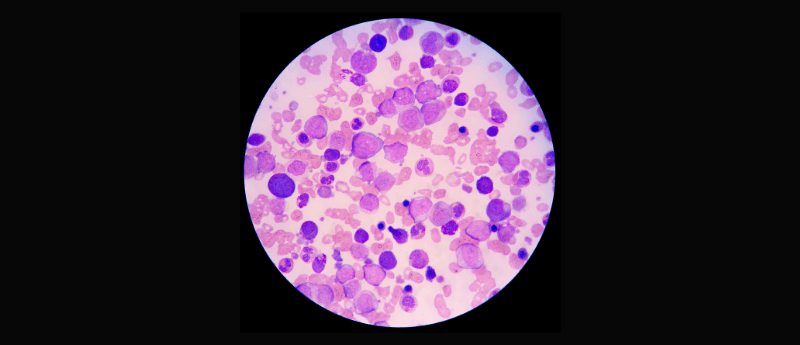
AML is an aggressive form of blood cancer affecting a group of white blood cells (monocytes and granulocytes) called myeloid cells. As the most aggressive and one of the most common types of leukemia, AML develops very quickly and requires urgent treatment. Chemotherapy is the main treatment for AML, but unfortunately, the disease has a poor prognosis due to a high relapse rate.
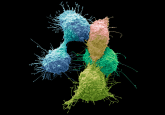
In recent years, CAR T-cell therapy has shown promise in treating relapsed leukemias, and it targets tumors with more precision than chemotherapy. CAR T-cell therapy harnesses the body’s own immune system to target cancer cells more effectively, through reprogramming a patient’s immune cells to target a cancer-specific protein.
However, the effectiveness of CAR T-cell therapy can be hampered by cancer cells that evade detection due to the absence of the targeted protein, leading to relapse. The St. Jude team sought to overcome this challenge by targeting two different cancer-related proteins simultaneously. Where others have previously failed due to the bispecific structure of CAR, here the team adopted an innovative approach by modifying the CAR T cells with an additional binding domain for the second targeted protein.
“The two different binding domains of the CAR are like having two barcode scanners instead of one, looking for their appropriate barcode, the targeted cancer-related proteins,” senior author Paulina Velasquez explained. “Normally, a CAR has a single barcode scanner. Here, we placed two slightly different barcode scanners on top of each other, and if either one detects an appropriate target barcode, the anti-cancer immunotherapy response activates.”
The team leveraged AI-based modeling tools, including AlphaFold predicted protein structures, to optimize their design. By analyzing structural components and linker flexibility, they identified key factors influencing therapeutic efficacy.
The dual-targeted CAR T cells demonstrated superior performance in both lab experiments and animal models, offering hope for improved treatment outcomes.
This research not only advances CAR T–cell therapy for childhood leukemia but also emphasizes the potential of AI tools in improving personalized cancer treatment. As co-author Kaylan Immadisetty concluded, “Most importantly, others can now use our computational approach for designing their CARS. And hopefully, it will help them understand the efficacy of their CAR technology and lead to overall improvements for leukemia and other malignancies.”