Particle Uptake in Cancer Cells to Predict Malignancy and Drug Resistance
Following an arc of discoveries regarding the mechanical properties of cancer cells, a research team from The Hebrew University (Jerusalem, Israel) has developed a groundbreaking new method to classify cancer cells by their ability to internalize particles of various sizes.
Cell biomechanics, including properties such as cytoskeletal structure and membrane fluidity, significantly influence cellular functions like mobility, invasion, and metastasis, which are critical in cancer progression.
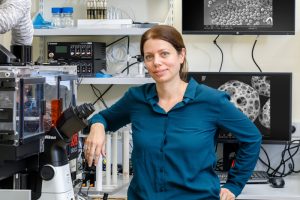
Ofra Benny- Principle Investigator of Benny Lab for Nanomedicine & Tumor Microenvironment
The research team, led by Ofra Benny, had been exploring such properties in their work, and found strong correlations between higher cell elasticity and higher malignancy levels.
The elasticity of a cell’s membrane in turn correlates with its ability to uptake external material. If the membrane is more elastic, it is easier for it to envelop this material.
With this in mind, the team wondered whether it would be possible to measure uptake in cancer cells, using it as a proxy for elasticity to classify them.
They analyzed three pairs of human cancer cell subpopulations with differing levels of drug resistance or malignancy. The cells were incubated with fluorescently labeled polystyrene particles of various sizes and their uptake patterns were measured using flow cytometry.
Termed ‘Mechanomics’, their method uses particle uptake measurements and a number of explainable AI algorithms to classify cancer cells based on their ability to internalize particles of various sizes.
Opting for an explainable AI approach, the team utilized three algorithms to classify cancer cells: the support vector machine, random forest, and XGBoost. Using these in combination they were able to classify cancer cell subtypes with accuracy rates exceeding 95%.
Their mechanomics approach shows promise in accurately predicting cancer cell phenotypes, even in morphologically similar cells, suggesting potential clinical applications for personalized therapy and improved patient outcomes. This is something Ofra and her team are actively exploring in collaboration with a nearby hospital.
Importantly, the study’s findings also shed new light on the importance of integrating mechanical and phenotypic data to advance cellular medicine.
Stay tuned for a brilliant interview coming up soon with Ofra Benny where we discuss the fascinating story of this discovery.